According to the American Cancer Society, cervical cancer was once one of the most common causes of cancer death among women in the U.S. Increased screening via Pap smears caused the number of deaths to drop dramatically. Human papillomavirus vaccines are also helping: According to the Centers for Disease Control and Prevention, “clinical trials showed HPV vaccines provide close to 100% protection against cervical precancers and genital warts.” We spoke with Dr. Valentin Kolev, a gynecologic oncologist at the Blavatnik Family – Chelsea Medical Center at Mount Sinai, for more information.
Protect yourself from cervical cancer

Photo: iStock.
What is cervical cancer?
Cervical cancer is cancer arising from the cervix, which is the lowest part of the uterus that connects to the vagina. Cervical cancer is one the most easily diagnosed and regularly screened types of gynecologic cancer.
What are the symptoms?
Early on, typically no symptoms are seen. Later symptoms may include abnormal vaginal bleeding, pelvic pain, pain during intercourse, vaginal discharge, or bleeding after sexual intercourse.
What are the risk factors of cervical?
Most of the risk factors for cervical cancer are associated with an increased risk of acquiring or having an appropriate immune response to infection with HPV. These include early onset of sexual activity, multiple sexual partners, a high-risk sexual partner (partner with multiple sexual partners or HPV infection) and immunosuppression (HIV, immunosuppressive therapy).
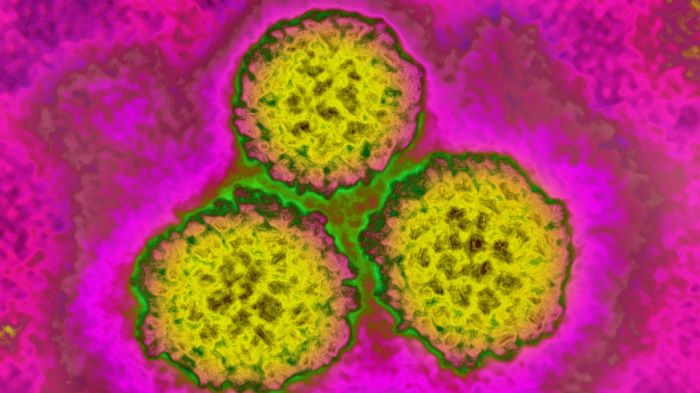
What is HPV?
Human papillomavirus (HPV) is a group of more than 100 different viruses. It is the most common sexually transmitted infection. Some of the viruses can cause skin warts or cancer of the mouth/throat, anus/rectum, or cervix in women and penis in men. Nearly all cervical cancer can be attributed to HPV infection.
If I have HPV, what are the odds of developing cervical cancer?
Most cervical HPV infections are transient and occur in young women. Eighty to 90% of new HPV infections will resolve within two years. A small proportion of infections with certain types of HPV can persist and progress to cancer.
While HPV is responsible for most cervical cancers, what other factors play a role (genetics, etc.)?
There is no well-established model of the genetic basis for cervical cancer. Oral contraceptives and cigarette smoking both have been associated with an increased risk of developing cervical cancer in people infected with the HPV virus.
How can I lower my risk?
The primary prevention of cervical cancer is a vaccination against the high-risk HPV infection and having routine screening. Other ways to decrease the risk is by using barrier protection and spermicides with intercourse.
What does screening entail? How often should I be screened for cervical cancer?
Screenings for cervical cancer should start at 21 years of age regardless of the age of initial sexual activity. The screening is part of Gynecologic examination where cells are taken from the cervix. Cells are removed from the cervix with a brush or other sampling instrument.
• Women aged 21–29 years should have a Pap test alone every three years. HPV testing is not recommended.
• Women aged 30–65 years should have a Pap test and an HPV test (co-testing) every five years (preferred). It also is acceptable to have a Pap test alone every three years.
The HPV vaccine is marked toward preteens and teens. Is there any value to getting vaccinated if you are older?
It is recommended to get the vaccine before the age of 15. Recently FDA approved the vaccine administration for adults up to the age of 45. That was based on a study of 3,200 women. The vaccine was 88% effective in preventing persistent infection, genital warts, precancerous lesions of the cervix, vulva or vagina, and cervical cancer.
How is cervical cancer treated?
The treatment of cervical cancer is dependent on the stage. It may include surgery or radiation with chemotherapy. If the disease is caught early there are options for fertility preservation with removing only the portion for the cervix or the whole cervix and preserving the uterus.