February, the month of Valentine’s Day, is also, fittingly, American Heart Month. Most people know this, thanks to numerous awareness campaigns and activities like walks and other fundraisers. What people might not know is that while heart disease is the leading killer for all Americans, African-Americans and Hispanics face even greater risks. We talked to Dr. Annapoorna S. Kini, a cardiologist at the Mount Sinai Hospital, to learn about what’s behind the statistics.
Why blacks and Hispanics are at higher risk of heart disease
Photo: iStock
What is the risk of heart disease among African Americans and Hispanics in this country?
The prevalence of high blood pressure in African-Americans is the highest in the world. Research suggests African-Americans may carry a gene that makes them more salt-sensitive, increasing the risk of high blood pressure and heart disease. African-Americans are disproportionately affected by obesity. Among non-Hispanic blacks 20 and older, 63 percent of men and 77 percent of women are overweight or obese. African-Americans are more likely to have diabetes than non-Hispanic whites.
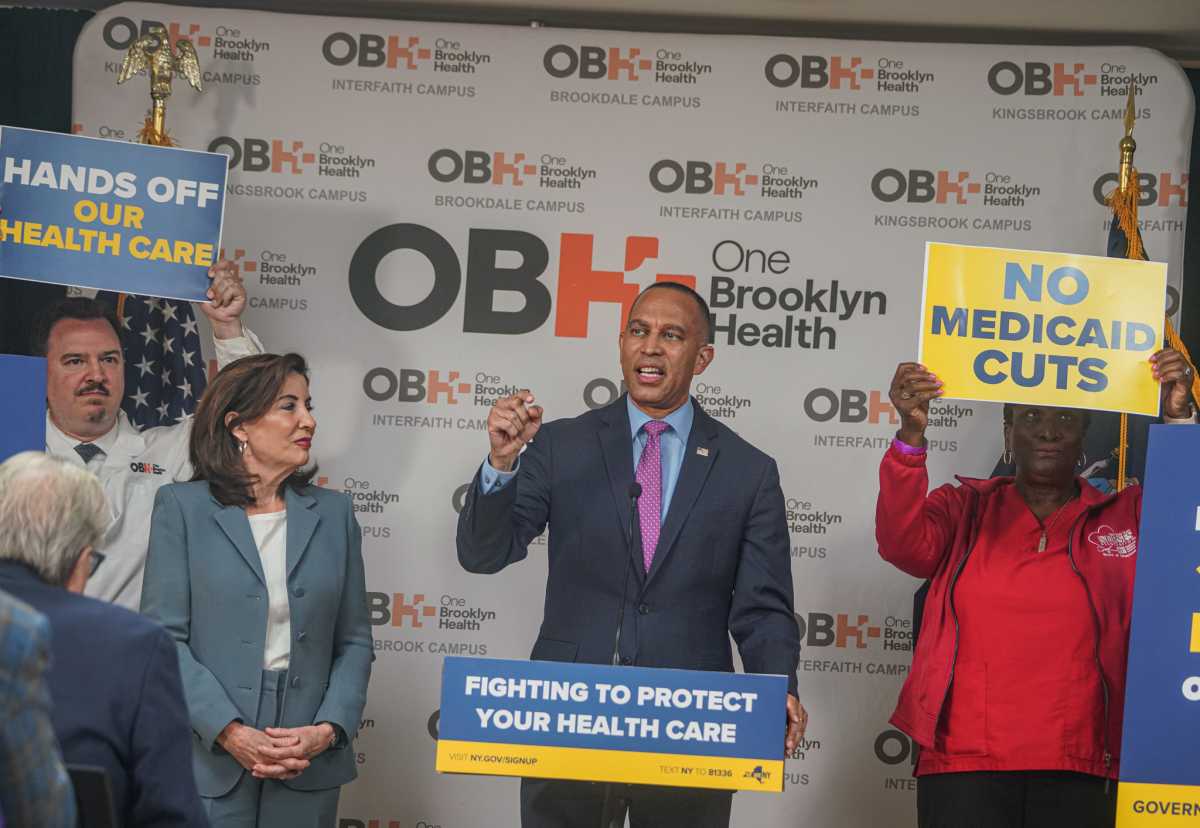
The American Heart Association recently issued a scientific statement highlighting the public health burden of cardiovascular disease in Hispanics and calling for the development of culturally tailored interventions and the prioritizing of Latinos in the nation’s heart-health-improvement goals. An underlying issue is the acknowledgment of an insufficient understanding of Hispanic heart health in general and specifically with respect to differences by Hispanic background, particularly in terms of demographic characteristics, sociocultural factors, diet, and health behaviors.
Are the risks different for men and women among African-Americans and Hispanics?
Rates of hypertension in the community and in stroke populations have been higher in black women than in black men in some studies. Other data suggest that hypertension confers a higher risk for stroke in black women than black men, although both are at high risk. In our study, we found sex differences in frequencies of hypertension. Differences in pathophysiology, severity, treatment of hypertension, or psychosocial factors may account for the observed sex difference. African-American women may have a greater risk of stroke from hypertension and other risk factors than their male counterparts.
What should people at risk do to prevent heart disease? Are there extra precautions for populations at greater risk?
Lifestyle modifications and decrease weight: Diet changes like eliminating sugary drinks and desserts, making vegetables and white meat the main part of the meal and walking at least 30 minutes a day help.
When should people in higher risk groups start getting screened for heart disease?
High blood pressure and high cholesterol can damage your heart and blood vessels. But without testing for them, you probably won’t know whether you have these conditions. Regular screening can tell you what your numbers are and whether you need to take action:
● Blood pressure. Regular blood pressure screenings usually start in childhood. You should have a blood pressure test performed at least once every two years to screen for high blood pressure as a risk factor for heart disease and stroke, starting at age 18.
If you’re age 40 or older, or you’re between the ages of 18 and 39 with a high risk of high blood pressure, ask your doctor for a blood pressure reading every year. Optimal blood pressure is less than 120/80.
● Cholesterol levels. Adults should generally have their cholesterol measured at least once every five years starting at age 18. Earlier testing may be recommended if you have other risk factors, such as a family history of early-onset heart disease.
● Diabetes screening. Since diabetes is a risk factor for developing heart disease, you may want to consider being screened for diabetes. Talk to your doctor about when you should have a fasting blood sugar test or hemoglobin A1C test to check for diabetes.
● Depending on your risk factors, such as being overweight or having a family history of diabetes, your doctor may recommend early screening for diabetes. If your weight is normal and you don’t have other risk factors for type 2 diabetes, the American Diabetes Association recommends starting screening at age 45, and then retesting every three years.
If you have a condition such as high cholesterol, high blood pressure or diabetes, your doctor may prescribe medications and recommend lifestyle changes. Make sure to take your medications as your doctor prescribes and follow a healthy lifestyle plan.
What are some signs/symptoms that you shouldn’t ignore?
Chest discomfort, nausea, indigestion, heartburn, or stomach pain; pain that radiates to the arm; dizzy or lightheadedness; throat or jaw pain; becoming exhausted easily; excessive sweating; a cough that won’t quit; swollen legs, feet, and ankles; irregular heartbeat.