(Reuters) – U.S. doctors running out of narcotics needed for COVID-19 patients on ventilators are asking the federal government to raise production limits for drugmakers, according to a letter seen by Reuters, after national quotas had been tightened to address the opioid addiction crisis.
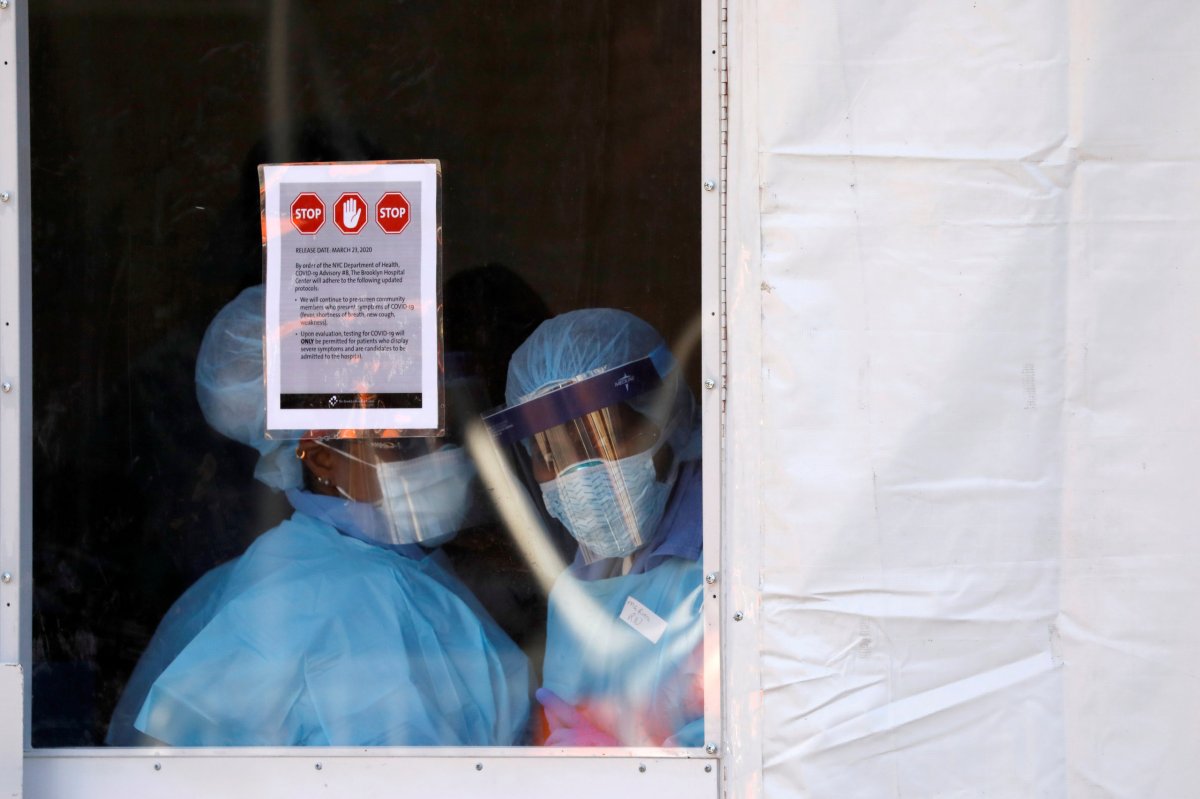
The global coronavirus pandemic has led to more than 5,300 deaths nationwide, with over 227,000 confirmed cases, according to a Reuters tally, and has sent states and the federal government scrambling to obtain enough ventilators to treat patients struggling to get oxygen.
At the same time, hospitals are churning through drugs, including injectable fentanyl, used to safely place patients on ventilators and keep them sedated so their lungs can heal.
The U.S. government sets annual limits on how much tightly regulated narcotics can be produced by pharmaceutical companies, and then allocates portions to various manufacturers. Amid an outcry over opioid abuse, the U.S. Drug Enforcement Administration (DEA) reduced the overall fentanyl quota by over 30% for 2020.
In a letter to the DEA on Tuesday, groups including the American Medical Association and the American Society of Health-System Pharmacists (ASHP) said supplies of injectable fentanyl, morphine and hydromorphone are already in short supply and asked for increased company allocations.
“We appreciate DEA’s work to protect against diversion and maintain control over the flow of opioids into our communities,” they wrote. “However, during this unprecedented health crisis, hospitals must have sufficient (drug) supply to treat patients.”
A senior DEA official told Reuters the agency currently believes the existing national quotas are “completely sufficient” to meet the spike in demand, and there is still room for additional allocations to companies under the cap to make millions more injectable doses that hospitals use.
The agency is closely monitoring the situation, however, and has begun discussing steps it can take to expedite an overall quota hike if necessary, the official, who asked to remain anonymous, said.
“These are unprecedented times, and the DEA is taking unprecedented actions to make sure we support hospitals on the front lines,” the official said.
In a statement, Pfizer Inc <PFE.N> said it adjusted production schedules to prioritize injectable fentanyl in high demand. The DEA raised the company’s quota this week, it said.
U.S. hospitals are currently projected to need about 40,000 intensive care beds to treat patients with COVID-19, the highly contagious respiratory illness caused by the virus, according to the Institute for Health Metrics and Evaluation at the University of Washington. That could lead to a shortage of nearly 20,000, IHME said.
Nearly 32,000 ventilators may be needed, IHME said, although Governor Andrew Cuomo has said New York alone may need 30,000 to address the expected spike in cases in coming days and weeks at the outbreak’s current epicenter.
Doctors and nurses can use a range of drugs to help patients that need a ventilator. Some, such as anesthesia drug propofol, are not as tightly regulated as opioids like fentanyl. But hospital staff around the country have already begun reporting shortages of many of these drugs, and difficulty filling orders.
Demand for fentanyl, hydromorphone and morphine spiked 67% in March compared to January, according to Vizient, which helps healthcare providers manage their supply chains. At the same time, the fill rate for Vizient members had dropped to 73% by March 25.
‘A VERY SERIOUS ISSUE’
Dr. Michael Ganio, director of pharmacy practice and quality at ASHP, said doctors will be forced to use different and less common combinations of sedatives if shortages continue to mount. That increases the risk of medical errors, he said.
The DEA last week agreed to relax inventory controls for manufacturers, allowing them to produce and store more than 65% of their annual quota throughout the duration of the emergency.
“This exception does not authorize any manufacturer to exceed his previously established annual manufacturing quota,” the DEA wrote.
The U.S. Department of Health and Human Services issued a request for information from drug manufacturers this week on their ability to rapidly produce the maximum number of ventilator medicines, with various quantity and price scenarios.
“The United States has a critical need to procure priority medicines for ventilated ICU (intensive care unit) patients in response to COVID-19,” it said.
Patients may receive paralyzing drugs, in addition to sedatives, to increase the ventilator’s effectiveness. If the sedatives are not effective, a patient could potentially gain consciousness but be unable to alert medical staff.
“It keeps me up at night,” Ganio said. “This is a very serious issue we’re seeing.”
(Reporting by Dan Levine in Oakland, California; Editing by Bill Berkrot)