(Reuters) – As the coronavirus pandemic spreads deeper into America’s small towns and rural outposts, Dr. Tallulah Holmstrom has seen familiar faces fill her intensive-care unit in Camden, South Carolina.
A native of this hamlet of 7,000 people, Holmstrom saw its ICU threatened with closure in recent years as specialists departed for bigger cities. Now faraway doctors are helping treat the community’s COVID-19 patients, thanks to technology.
KershawHealth, the local hospital, installed cameras and other equipment for 24-hour monitoring by a company that employs doctors and nurses remotely. Sitting in cubicles in St. Louis, Houston and Honolulu, as well as other countries including Israel and India, these medical workers watch patients’ vital signs on computer screens and talk to local staff on two-way video about medications and treatments. KershawHealth employees can summon emergency help from these teleworkers by hitting a button on the wall.
Holmstrom said those changes, begun four years ago, have helped her hospital better handle the current crisis. While Camden and surrounding Kershaw County have seen more than 1,600 confirmed infections and 34 deaths, the technology has enabled many of the area’s COVID-19 patients to be hospitalized close to home.
“Now a patient can look up from their ICU bed here and they are seeing a friend’s daughter or son taking care of them or someone they go to church with,” said Holmstrom, chief medical officer at KershawHealth.
Camden is among a growing number of communities relying on this elaborate form of telemedicine to cope with an unrelenting COVID-19 case load and to manage unpredictable surges.
Well before the current crisis, vast stretches of rural America lacked easy access to advanced medical care. More than 130 rural hospitals have closed in the United States since 2010, including 18 last year, according to University of North Carolina researchers.
Rural areas tend to have higher rates of underlying health conditions such as diabetes and hypertension. Their populations often are older and poorer – making them more vulnerable to COVID-19.
Even if beds were available, qualified staff are hard to find. It’s estimated that 43 states, including South Carolina, face a shortage of highly trained ICU doctors, known as intensivists, according to researchers at George Washington University. These shortages may worsen with hospitalizations in many states predicted to peak this fall, when the coronavirus mixes with flu season, according to Patricia Pittman, director of the university’s Mullan Institute for Health Workforce Equity.
“No one is suggesting telemedicine is ideal, but it’s probably one of the least bad options,” she said. “It is definitely better than having no one and helicoptering people out.”
SCALING EXPERTISE
About a third of U.S. hospitals surveyed in 2017 said they had access to a formal program of telemedicine for critically ill patients. Studies have shown telemedicine can benefit ICU patients by promoting the best practices supported by medical evidence and by reducing complications. During the pandemic, doctors say, it has helped conserve personal protective equipment and reduce workers’ exposure to the virus.
There can be drawbacks, too, if physicians try to monitor too many people at once, which can lead to poor decisions or even medical errors. Tele-ICU generally requires physicians working remotely to hold a license in each state where people are hospitalized.
The Trump administration has eased rules on telehealth during the pandemic and expanded reimbursement by Medicare. Shares of telemedicine companies such as Teladoc Health Inc have soared as patients embraced online visits.
Sutter Health, a large hospital system in California, said it manages more than 300 ICU beds across 18 hospitals from offices in Sacramento and San Francisco.
Earlier this month at its Sacramento hub, Dr. Vanessa Walker checked in remotely on a patient who was taken off a ventilator earlier in the day at Sutter’s Roseville hospital about 25 miles away. Using a headset and camera, she clicked the patient’s name on her screen, which rang a doorbell to notify the patient that she was entering the room via video.
“Save your breath. You’re doing well otherwise,” she told the patient.
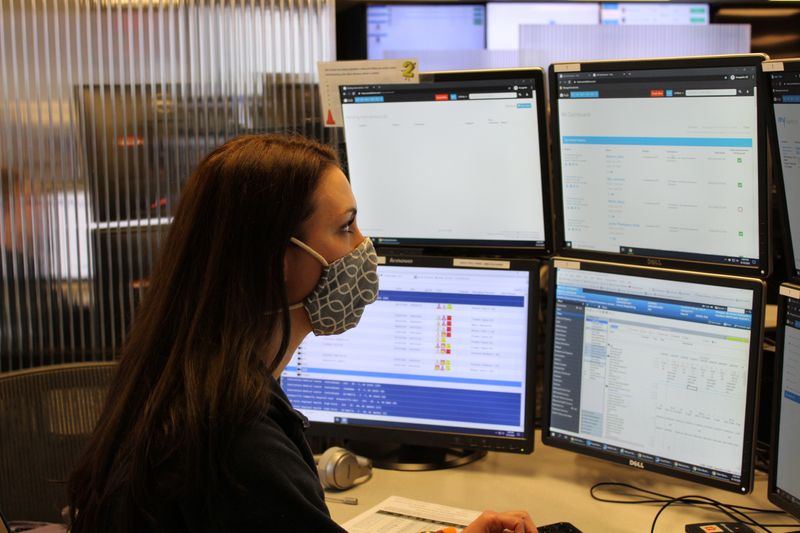
Walker, the medical director of Sutter’s electronic ICU for its hospitals in California’s Central Valley, had a wide array of information across six monitors at her desk. She could review medical records and see multiple scans of the patient’s lungs before and after treatment.
CAUTIONARY TALE
As use of this technology grows, patient-safety advocates warn hospitals not to cut corners. They say cameras and computers are no substitute for trained professionals at the bedside who can respond rapidly to life-threatening complications.
The Leapfrog Group, a nonprofit that monitors patient safety, recommends that a physician certified in critical care medicine perform an in-person review of each ICU patient daily before handing off monitoring to colleagues remotely. The group says remote doctors should lower their patient loads if they can’t respond within five minutes to requests from on-site staff and evaluate the patient.
Steve Burrows, a Los Angeles filmmaker, remains a skeptic.
He said his mother had complications during a hip operation in 2009 and suffered permanent brain damage in surgery and the ICU at a Wisconsin hospital.
In litigation, Burrows said, he learned that a doctor was remotely monitoring more than 150 ICU patients, and there was no physician in the ICU who could respond to his mother’s low blood pressure. He released an HBO documentary, “Bleed Out,” in 2018 about his mother’s case.
“Telemedicine is fantastic if it’s used properly,” he said in an interview. “But I think replacing doctors at the bedside with technology is insane.”
At trial, a jury found there was no negligence by the hospital. Advocate Aurora Health, the current hospital owner after a merger, said its electronic ICU “does not replace bedside caregivers. Instead, it serves as an additional set of eyes that provides an extra layer of safety.”
‘CONSTANT ATTENTION’
Advanced ICU Care, the St. Louis company serving Camden, works with more than 90 hospitals in 26 states. Overall, it has treated more than 1,300 COVID-19 patients.
“These patients need constant attention and continuous adjustments. That is a lot of what we do,” said Dr. Ram Srinivasan, the company’s chief medical officer.
South Carolina remains a hot spot for coronavirus infections with more than 126,000 cases and 2,877 confirmed deaths as of September 11.
The state’s first two cases of COVID-19 were announced the same day in early March and one was in Camden, a place so rural that signs remind people not to ride horses on the sidewalk.
Holmstrom, the chief medical officer at KershawHealth, got a call with the news while driving home that Friday, March 6. Within a matter of days, there were six people infected and four were hospitalized.
The Camden ICU was nearly full for weeks as the medical staff juggled COVID-19 patients alongside the normal flow of critically ill people. Hospitalizations eased around Memorial Day, Holmstrom said, only to surge again in July and much of August.
“When you’re a town this small and 32 people get sick in one day that’s a lot,” said Vic Carpenter, Kershaw County administrator.
Holmstrom, who was born in the hospital where she now works, has experienced highs and lows. A close friend who spent six weeks in the hospital is now back to full strength. Holmstrom arranged final video calls for others to say goodbye to their families.
KershawHealth is bracing for another surge this fall, when it once again will turn to remote doctors to back up busy hospital staff.
“It’s like someone constantly in the background overlooking everything with your care,” Holmstrom said.
(Reporting by Chad Terhune in Los Angeles; Additional reporting by Nathan Frandino in Sacramento; Editing by Marla Dickerson)