MILTON KEYNES, England (Reuters) – At Milton Keynes University Hospital in England, it’s a battle between life and death. For those most ill, death is gaining the upper hand.
The latest COVID-19 wave has hit the hospital northwest of London with even more force than the first: younger patients fill its wards and fewer of the sickest people respond to treatment.
Doctors and nurses are grappling with the strain of exhaustion and loss.
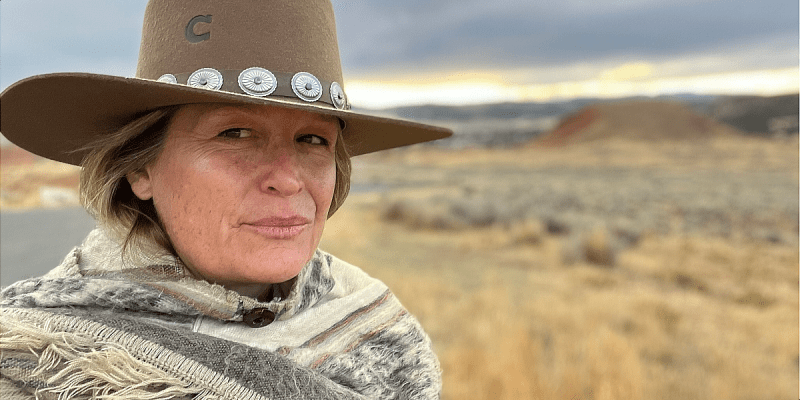
Joy Halliday, consultant in intensive care and acute medicine, is in charge of a high-dependency unit for COVID-19. It is a step down from an intensive care unit (ICU), and severely ill patients there are receiving CPAP oxygen.
Stephen Marshall, 68, is one of them. After testing negative for COVID-19 following a recent operation on his back, he initially thought he had a cold.
“I should never have left it, it’s just made it worse,” he said, speaking through a mask pumping oxygen into his lungs.
“I’m on oxygen all the time now,” he said. “I seem to be holding my own at the moment, so touching wood,” he added, lifting his hand to his head.
Halliday said that with visits curtailed, the doctors and nurses were supporting patients emotionally as well as medically.
“I can only just imagine how difficult that is for family at the end of the telephone to be told that their loved one is getting worse … or they’re agitated or their oxygen levels are dropping,” she said.
“It’s difficult for us to see and it’s even more difficult for them.”
The youngest person in her eight-bed unit is 51-year-old supermarket worker Victorita Andries. She was put on oxygen immediately when she was admitted five days ago.
“The machine for me has been good,” said Andries, adding that she felt positive about the future. The oxygen levels in her mask are gradually being reduced as her condition improves.
The youngest person being ventilated in the hospital is just 28.
The official death toll from COVID-19 in the United Kingdom is 93,290, the highest in Europe and the fifth worst in the world after the United States, Brazil, India and Mexico. 39,068 COVID-19 patients are being treated in hospitals. Deaths rose by a record 1,820 people on Wednesday.
INTENSIVE CARE
In the ICU, where all seven patients had COVID-19, the quiet is interrupted by machines bleeping and oxygen pumping.
Wassim Shamsuddin, clinical director for anaesthesia and intensive care, said the patients were receiving mechanical ventilation, which requires sedation.
“This time around what we’re finding is that patients aren’t faring as well if they need to be invasively ventilated,” he told Reuters.
“Our mortality probably in the first wave for patients coming onto intensive care was around 40%. This time around we find that the mortality is about 80%.”
He explained that unlike in the first wave, all COVID-19 patients in the hospital now automatically receive remdesivir and dexamethasone after they were found to be effective.
That means that those who end up in ICU during the second wave of the pandemic are more likely to be the sickest patients, because they have not responded to those treatments.
Shamsuddin added that he did not know whether a highly transmissible new variant of the disease found in the UK also contributed to higher death rates.
He said intensive care staff, who have been boosted by medics and nurses from other wards during the pandemic to maintain one-on-one care, were not used to such high levels of death.
“At the moment we’re just all keeping our heads down and just getting on with it,” he said.
“Intensive care hospitals are meant to be a place where we treat patients and make them better. The difficulty here is that even though we try our best and we throw everything at the patients, it just doesn’t seem to be working.”
‘DEATH EVERY DAY’
Joe Harrison, chief executive of Milton Keynes University Hospital NHS Foundation Trust, said the hospital had seen more than twice the number of patients in the second wave than the first, and currently had 186 patients with COVID-19.
“We believe that over the next week or so, we’re going to continue to see real pressures in our critical care unit,” he said. “And then hopefully we will turn the corner and things will start to improve.”
He found it “absolutely inspirational” to see how the medical staff had dealt with the pressures that COVID-19 had brought since it first surfaced in the country early last year.
Back in the high-dependency unit, Halliday and other staff managed to forge close bonds with the patients, despite having to wear full protective gear and interact from behind masks and visors.
Patient Geoffrey Winter, aged 70, called the care he had received “fantastic”.
“Two of the nurses were cleaning my feet this morning; I felt like Jesus,” he joked.
But Halliday echoed the view that it was tougher this time around.
“It’s draining. It’s draining physically. It’s draining mentally,” she said.
“It’s difficult to keep going on a day-to-day basis for staff, just to see death in death out, every day.”
(Reporting by Paul Sandle; Editing Guy Faulconbridge and Mike Collett-White)