LOS ANGELES (Reuters) – A former Arkansas health official is sounding alarms about the pace of coronavirus vaccines being administered to residents of long-term care facilities under a U.S. plan that puts major pharmacy chains CVS and Walgreens in charge of many of the shots.
Fewer than 10% of doses allocated to those Arkansas seniors have been administered, according to the state health department. The two pharmacies are working with about 40% of the state’s facilities. Some of those were told that they were scheduled for February or March, said Dr. Joe Thompson, former Arkansas surgeon general and chief executive of the Arkansas Center for Health Improvement
“This is not acceptable,” said Thompson. “We’re seeing a failure in deployment by CVS and Walgreens.”
Federal health officials in recent days have urged broadening vaccine eligibility to tens of millions of Americans to speed the national inoculation program rollout. Meanwhile, seniors at some long-term care facilities – who account for about 1% of the U.S. population but 40% of COVID-19 deaths and were supposed to be at the front of the line – continue to wait.
State and local officials and long-term care operators in states including Florida, California, Arizona, Indiana and Pennsylvania told Reuters they have turned to alternative providers for vaccinations for their residents or staff because the pharmacy chains were scheduling shots weeks out.
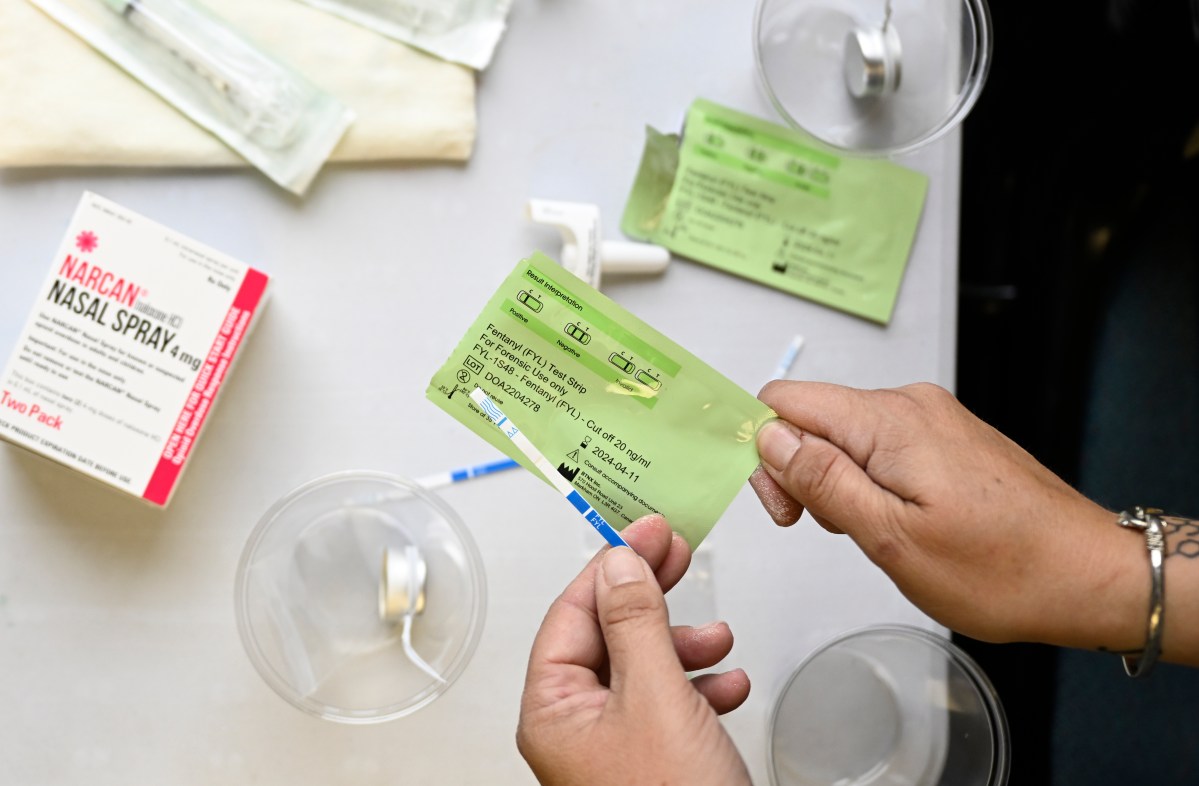
Some 75,000 long-term care facilities signed up to receive vaccines from CVS Health Corp and Walgreens Boots Alliance Inc under the U.S. Centers for Disease Control and Prevention’s (CDC) Pharmacy Partnership Program.
“I think they face serious bandwidth issues in terms of scheduling,” said David Grabowski, a Harvard Medical School professor and healthcare policy expert. “I find it very distressing that we haven’t been doing this more rapidly. This is really a matter of life or death.”
Arkansas Governor Asa Hutchinson in a statement on Thursday said the two pharmacy chains assured him that all long-term care residents assigned to them would be vaccinated by the end of this month.
Many states prioritized homes with patients requiring medical care, which contributed to delays at other long-term care facilities.
CVS said it plans to finish all shots at assigned facilities within nine to 12 weeks of the first dose. That means states like California, Florida, Arizona, Alabama, Oklahoma and Pennsylvania, which were among the last to activate the second-phase of facility vaccinations, may not be finished until April.
“State decisions on which facilities are activated when have a significant impact on timing,” CVS spokesman T.J. Crawford said, noting that the company has administered 1 million shots and is on track with its federal agreement.
Others hurdles included confirming vaccine availability, the winter holidays, vaccine hesitancy and fresh COVID-19 outbreaks, the companies said.
That resulted in “a little bit slower start than what we were hoping for. Now that we’ve gotten past the first of the year, you’re seeing a quick and rapid acceleration,” said Rick Gates, Walgreens’ senior vice president of pharmacy and healthcare. The company has done more than 500,000 shots and expects to be done by March.
‘OVERWHELMED BY THE SHEER VOLUME’
Meanwhile, central Florida’s Seminole County is deploying mobile clinics to some assisted living facilities.
“We went because they either have not been contacted by the private providers or they had concerns because of some type of issue,” said county emergency manager Alan Harris.
“CVS and Walgreens, I think, are overwhelmed by the sheer volume of long-term care facilities in Florida,” Harris said.
The state of Florida has hired health services firm CDR Maguire to take over vaccinations at about 1,900 assisted living facilities that CVS or Walgreens had scheduled on or after Jan. 24.
Los Angeles County opted out of the CVS-Walgreens partnership and is asking facilities that can to pick up and administer vaccine themselves. In Northern California’s Contra Costa County, nonprofit Choice in Aging joined John Muir Health and Kaiser Permanente in pitching in to help.
Choice in Aging is targeting facilities with six or fewer beds in historically underserved communities. “This is a population that is never prioritized,” said Choice in Aging CEO Debbie Toth.
The CDC on Thursday said 26% of the 4.7 million vaccine doses allocated for long-term care sites had been administered, lagging even the woeful 36% of the 30.6 million available nationwide.
Graphic: Vaccine rollout in nursing homes – https://graphics.reuters.com/HEALTH-CORONAVIRUS/VACCINES-NURSINGHOMES/jznvnmbwnpl/chart.png
West Virginia, which opted out of CDC Pharmacy Partnership, did extensive planning and tapped its existing network of long-term care pharmacies to quickly vaccinate nursing home residents in an all-hands-on-deck effort, said Dr. Michael Wasserman, former president of the California Association of Long Term Care Medicine.
“Community pharmacies absolutely should be involved,” said American Pharmacists Association CEO Scott Knoer. “I wish they would have been from the get-go.”
(Reporting By Lisa Baertlein and Deena Beasley; additional reporting by Carl O’Donnell in New York; Editing by Peter Henderson, Bill Berkrot and Jonathan Oatis)